
It’s not easy watching your dog grow old. Their steps become slower. Their joints get stiff or fail them. Their eyes fail them. Their hearing fails them. All age related issues you see in geriatric humans, you’ll see in your canine family member. You become acutely aware that your time together is shortening, and you deny to yourself that they’re a step closer to their final days, but you celebrate their age. she’s no longer 11, she’s “11 1/2”, she’s just “two months from 13”. Half-birthdays and extra months are celebratory events.
Rumble *13 in two months*, has never had an accident in the house, but did this past Saturday – Two times, within 5 minutes, then immediately went again outside. These were full-stream events. The next night, she peed and vomited in her crate during the night. Soooo…. That’s somewhat textbook for a urinary tract infection. Her urine was collected. How do we do that? Well, Rumble is a LOW squatter, so getting any urine from under her is impossible. We crated her, we lined her kennel with new clear plastic used to protect the floors for painting, or for covering plants, let her out after a hour in the crate, and into her plastic lined run, she goes, and we suck it up into a syringe. It helps us to get a clean (althought not sterile) urine catch. Off to the vet we go…
No, she’s not off her food [Rumble will eat up to the last minute of her life, I’m sure], and her behavior is normal. She has slowed down over the last month, and for the first time a few weeks ago, declined to chase a ball gently rolled for her to fetch. Her eyes are covered with old age cataracts. Her hearing is pretty good. She can absolutely hear the food bowls being readied. She does have some selective hearing – she loves to wander outside of the yard, and declines to hear me when I call her back. She’s a bit gimpy on one rear leg, following the gift of a body-slam from her granddaughter, and the subsequent CCL rupture, which we had repaired with a traditional ‘tight-rope’ sort of repair, using suture to create a make-do ligament. I would not put a nearly 12 year old through a TPLO, as the recovery is notable.
The vet checked the urine, which was amber colored and clear, only to find her urine tested clear of red blood cells, or leukocytes. A urinary analysis. checks for:
- color
- appearance (whether it is clear or cloudy)
- odor
- pH level (acidity)
- substances that are not normally in urine, such as blood, too much protein, glucose, ketones, and bilirubin
- cells, crystals, and casts (tube-shaped proteins)
- bacteria or other germs
Her U.A. showed nothing that indicated urinary tract infection. We agreed to send it in for a culture and sensitivity regardless, just in case we caught it very early, and a culture would allow bacteria that was not detected, to grow. Well, that was a surprise. We were pretty sure she’d have a urinary tract infection.
On to check the other organs! Her blood was drawn for a “senior panel”
Complete blood count (CBC) checks for
- total number of red blood cells (the RBC count)
- total amount of hemoglobin in the blood
- percentage of blood made up of red blood cells (the hematocrit)
- average red blood cell size (the mean corpuscular volume)
- average weight of hemoglobin per red blood cell (the mean corpuscular hemoglobin)
- average amount of hemoglobin per red blood cell (the mean corpuscular hemoglobin concentration)
- total number of white blood cells
- number of each type of white blood cell (the WBC differential), including neutrophils (the absolute neutrophil count, or ANC)
- number of platelets (the platelet count)
Biochemistry profile:
albumin, total protein, alkaline phosphatase, SGOT, SGPT, blood Urea, creatinine, bicarbonate (HCO3 ), chloride, sodium, potassium, calcium, phosphorus, cholesterol, glucose, lactate dehydrogenaseric acid.
A chemistry profile of various organs:
Liver Disease Markers For Liver Cell Injury Or Congenital Liver Disease:
Total Bilirubin., Alkaline phosphatase, SGOT and SGPT, Total protein, Albumin, LDH
Kidney Function Panel For Kidney Diseases:
Urea (Blood urea nitrogen), Creatinine, Electrolytes
Electrolyte Panel For The Status Of The Hydration Of The Body:
Sodium, Potassium, Chloride, CO2, and pH.
Thyroid hormone testing for Hypo Or Hyperthyroidism
Rumble’s Senior panel was perfectly normal. Her heart and lungs were normal. What are we left guessing if that culture and sensitivity come back normal? Probably canine senility, or cognative disorder, which is often demonstrated by a normally housetrained dog who suddenly starts having “accidents”; they signal less to go outside and may urinate or defecate indoors soon after being outside. This can progress to disorientation or confusion, disturbances of the sleep-wake cycle, decreased activity level, and sometimes less interaction/recognition of housemembers. She likely was aware that she had urinated in her crate that night, and this was stressful enough for her to cause her to vomit.

We’ll place Rumble on “Bright Mind” dog food, which, in our experience supports canine senior related cognative issues very well, and helps them with arthritic issues. We saw dramatic changes with Tank and Lucas. Hopefully this will help Rumble have a great quality of life. She’s still bright, healthy, and happy. That’s all we care about. Hopefully this diet will support the continuance of a happy life. We are likely just seeing the effects of age, which is a normal part of life. We’ll also have to pay more attention to her in the house, and get her out more regularly. She’ll likely need more baths if she has accidents in her crate, and beyond that, she’ll just live out her life as a well-loved old lady canine.






















 This is the radiologist’s review:
This is the radiologist’s review:
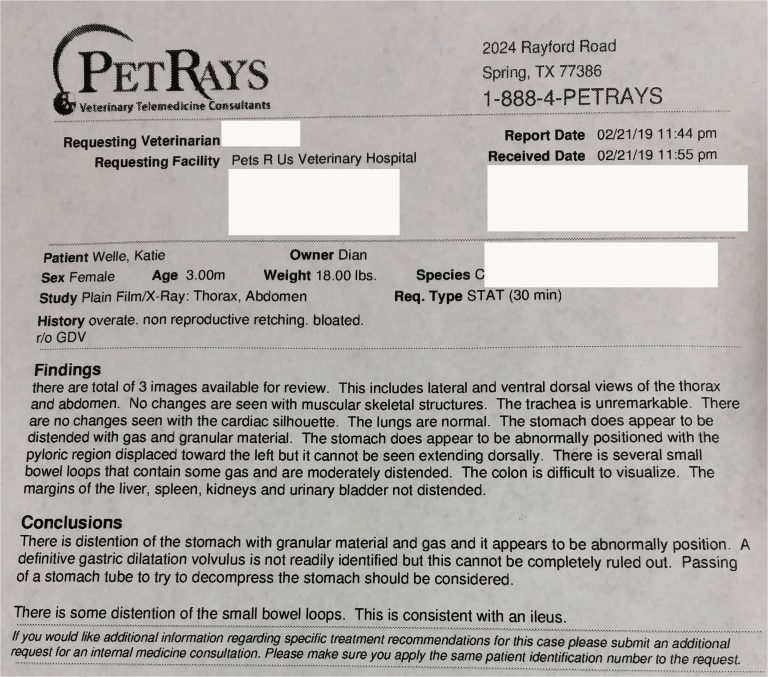 The Dr. told us to go home, and that he would call us the moment he finished the surgery. Reluctantly, we left our precious baby in his care, and prayed. We knew all the risks of this condition, and being a retired ER Nurse, I knew too much, which led me to believe I would never see Katie Bell alive again.
When the stomach twists, it immediately cuts off all circulation to the stomach and the bowels. The spleen is often involved in the torsion as well. Hemorrhage is a real risk when the spleen is damaged, and because the torsion has effects on the whole body, including the heart, the surgery and post-op period are gravely complicated. The risk of death is absolute in an adult dog (about 50% depending on the amount of time from torsion to surgery), and we were dealing with a baby. No veterinarian I have spoken to since, has ever seen GDV in a puppy, although literature states it can happen, and none would expect a puppy to survive.
Katie Bell was in the skilled hands of Dr. Habeeb, and absolutely was in the hands of God.
The Dr. told us to go home, and that he would call us the moment he finished the surgery. Reluctantly, we left our precious baby in his care, and prayed. We knew all the risks of this condition, and being a retired ER Nurse, I knew too much, which led me to believe I would never see Katie Bell alive again.
When the stomach twists, it immediately cuts off all circulation to the stomach and the bowels. The spleen is often involved in the torsion as well. Hemorrhage is a real risk when the spleen is damaged, and because the torsion has effects on the whole body, including the heart, the surgery and post-op period are gravely complicated. The risk of death is absolute in an adult dog (about 50% depending on the amount of time from torsion to surgery), and we were dealing with a baby. No veterinarian I have spoken to since, has ever seen GDV in a puppy, although literature states it can happen, and none would expect a puppy to survive.
Katie Bell was in the skilled hands of Dr. Habeeb, and absolutely was in the hands of God.
 The Dr. rotated her stomach back into position (yes, it was in full torsion), and her spleen and stomach were checked for damage. Her stomach was intact (no rupture), and as it re-profused, it looked like the tissue was going to be okay. Her spleen had a small amount of discoloration at the tip, but showed signs of re-profusion immediately. A tube was passed down the esophagus and into her stomach, to decompress the stomach, which was full of gas, fluid, and food. He did not surgically enter the stomach. A gastropexy was performed whereby the stomach is tacked to the body wall behind the rib cage down low, so that it could not twist again out of position, however, due to the delicate nature of her tissues, he was not confident that the gastropexy would hold. She did suffer some cardiac dysrhythmia related to decreased coronary perfusion and re-perfusion injury during the surgery.
A few hours later we got the call that she wasn’t just doing well, she was wagging her tail. He stated she was fully awake within 15 minutes of the surgery. Sedated, she would now sleep, and so could we. The next few days could bring heartache, as complications often happen within days of this surgery. Sometimes, the necrosis (death of tissue) is not fully realized when the surgery is complete, and death of stomach, bowel, heart, lung and spleen tissues could advance well after the surgery is complete.
Three days later, Katie Bell was released from the hospital. A good Veterinarian friend suggested human baby onesies, rather than make this baby wear a cone, as long as she did not fuss with the outfit. This was a precious tip! Not only was it effective, it was clean, and we bought several, so that they could be changed frequently, and darn it… they were darling.
We stayed with our daughter (in California) for a few more days, to be sure she would not suffer any complications, and because Katie Bell was on so many medications (about six), we wanted to make sure our trip home to Idaho was as risk-free as possible. I am very fortunate to have a number of friends who are Veterinarians, and breeder friends who have trusted vets, that we had the names of several who would see her at a moment’s notice, night or day, on our two day trip home. At least we thought it would be a two day trip home. We were wrong. A snow storm hit us when we reached Klamath Falls Oregon, and by the time we got to Bend Oregon, we knew we had to stay put. None of the Veterinarians we had lined up were in Bend. We took her to Central Oregon Animal Hospital and had her rechecked for safety by Dr. Douglas, wanting him to see her stable in the event she suffered any change in condition. What a kind and thoughtful Dr.!! She was in great condition (for a puppy who should have died), and we were much more comfortable knowing she had been rechecked. This was the second Veterinarian we had seen with her that was not familiar to us, which is scary when you have come to trust your pet to the care of well-vetted doctors.
We were snowed in for three days. We had her rechecked by her own vet the day after we got home. Needless to say, like the others, he just shook his head that this puppy was alive, and acting perfectly normal.
Katie is a *very* rapid eater, and immediately after surgery we realized the need for special bowls to slow her down.
The Dr. rotated her stomach back into position (yes, it was in full torsion), and her spleen and stomach were checked for damage. Her stomach was intact (no rupture), and as it re-profused, it looked like the tissue was going to be okay. Her spleen had a small amount of discoloration at the tip, but showed signs of re-profusion immediately. A tube was passed down the esophagus and into her stomach, to decompress the stomach, which was full of gas, fluid, and food. He did not surgically enter the stomach. A gastropexy was performed whereby the stomach is tacked to the body wall behind the rib cage down low, so that it could not twist again out of position, however, due to the delicate nature of her tissues, he was not confident that the gastropexy would hold. She did suffer some cardiac dysrhythmia related to decreased coronary perfusion and re-perfusion injury during the surgery.
A few hours later we got the call that she wasn’t just doing well, she was wagging her tail. He stated she was fully awake within 15 minutes of the surgery. Sedated, she would now sleep, and so could we. The next few days could bring heartache, as complications often happen within days of this surgery. Sometimes, the necrosis (death of tissue) is not fully realized when the surgery is complete, and death of stomach, bowel, heart, lung and spleen tissues could advance well after the surgery is complete.
Three days later, Katie Bell was released from the hospital. A good Veterinarian friend suggested human baby onesies, rather than make this baby wear a cone, as long as she did not fuss with the outfit. This was a precious tip! Not only was it effective, it was clean, and we bought several, so that they could be changed frequently, and darn it… they were darling.
We stayed with our daughter (in California) for a few more days, to be sure she would not suffer any complications, and because Katie Bell was on so many medications (about six), we wanted to make sure our trip home to Idaho was as risk-free as possible. I am very fortunate to have a number of friends who are Veterinarians, and breeder friends who have trusted vets, that we had the names of several who would see her at a moment’s notice, night or day, on our two day trip home. At least we thought it would be a two day trip home. We were wrong. A snow storm hit us when we reached Klamath Falls Oregon, and by the time we got to Bend Oregon, we knew we had to stay put. None of the Veterinarians we had lined up were in Bend. We took her to Central Oregon Animal Hospital and had her rechecked for safety by Dr. Douglas, wanting him to see her stable in the event she suffered any change in condition. What a kind and thoughtful Dr.!! She was in great condition (for a puppy who should have died), and we were much more comfortable knowing she had been rechecked. This was the second Veterinarian we had seen with her that was not familiar to us, which is scary when you have come to trust your pet to the care of well-vetted doctors.
We were snowed in for three days. We had her rechecked by her own vet the day after we got home. Needless to say, like the others, he just shook his head that this puppy was alive, and acting perfectly normal.
Katie is a *very* rapid eater, and immediately after surgery we realized the need for special bowls to slow her down.
















 I have had several new canine mothers with mastitis. For many years, the only thing I could do was apply ice packs or heat packs to give her relief, waiting for antibiotics to work. One day, I found another source of help…
I have had several new canine mothers with mastitis. For many years, the only thing I could do was apply ice packs or heat packs to give her relief, waiting for antibiotics to work. One day, I found another source of help…